WHAT IS PAP TEST?
The Pap test (Papanicolaou test), is also called the Pap smear or smear test. It is a simple test that scrapes cells off the surface of your cervix for examination in a laboratory.
WHY HAVE IT?
It can detect early warning signs of cancer of the cervix (cancer of the neck of the uterus). This is one of the most curable forms of cancer if detected early; hardly any women would die from it if all had regular Pap tests as recommended by the medical profession. Cervical cancer is related to exposure to the human papillomavirus (HPV or wart virus).
The early changes in the cells cause no symptoms, and the women in the early stages of cervical cancer feel quite healthy.
WHO SHOULD HAVE IT?
Any woman from 18 years of age who has had sex, including gay sex, should have a Pap test.
It should be performed after every 2 years AND up to the age of 69.
Even women who have stopped having periods or stopped having sex or have had the HPV vaccine should have regular Pap tests.
WHAT IS THE IDEAL TIME TO HAVE PAP TEST?
The best time to have a Pap test is any time after your period has finished. It should not be done if you have been douching or using vaginal tablets in the previous 48 hours.
You should wait for 34 hours after intercourse.
HOW IS THE PAP TEST DONE?
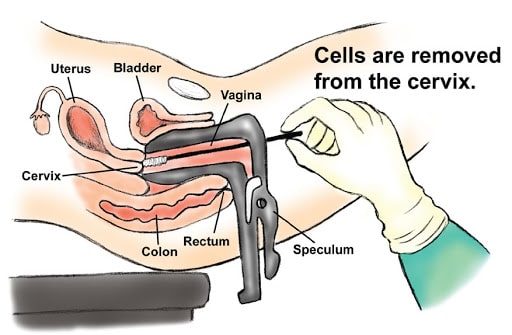
It is part of a normal pelvic or vaginal examination.
1. You lie on your back or your side on the couch.
2. An instrument called a speculum is slid gently into your vagina and then opened so that the doctor can see the cervix clearly, with the help of a light.
3. The smear is then taken with a thin spatula and a soft brush.
It is really a very thin amount of mucus with cells
that sit on the surface and the small opening of the cervix.
The smear is then placed on a glass slide, which is sent away to be tested.
Does the Pap test hurt or take long?
It is a simple test that does not take long (only about 2 to 3 minutes) and is uncomfortable, especially if you are tense, but should not cause any pain. The more relaxed you are the better. Deep breathing will help you relax.
WILL I FELL EMRASSED?
It is quite normal to feel a little embarrassed.
Doctors, of course, are used to doing these tests and perform many each day, so they understand.
Nobody has ever died of embarrassment, but many have died of cancer of the cervix by not having a Pap test.
WHAT ABOUT THE RESULT?
The results take about 1 to 2 weeks.
Ask your doctor when you should ring for the results. The results are almost always normal.
Abnormal cells are seen in only about 3 in 1000 tests and do not always mean cancer.
The microscopic findings are not infallible, unfortunately, but are improving all the time and are almost 100% accurate.
If there is any doubt, you will be recalled for a repeat test. For most women who have abnormal cells, the treatment is simple and effective.
WHAT ARE THE NEWER LABORATORY METHODS?
These are the Thin Prep and Papnet methods of studying the cells from the Pap test which is done in the usual way.
They appear to be better at picking up abnormal cells in doubtful cases but cost more.
However, the standard smear remains highly effective for screening
NOTE:
- A Pap test is simple, quick, and painless.
- It should be done every 2 years.
- It should be done throughout life from the start of sexual activity for up to 69 years.
- The test enables early detection of cell changes that could lead to cancer of the cervix.
- Cancer of the cervix is curable if detected early.
- The test is your safeguard